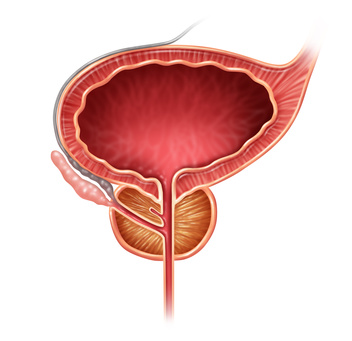

Prostate cancer is the most commonly diagnosed cancer in men and the second leading cause of cancer related deaths in the Western civilization. Although localized prostate cancer can be treated effectively by several curative therapies such as radical prostatectomy, conventional chemotherapies, external beam radiation therapy or brachytherapy, approximately 30-50 % of patients will have a local or distant recurrence. The majority of patients with metastatic disease initially respond to androgen deprivation therapy but, on average, the median survival for men with metastatic castrate resistant prostate cancer is 12 months. The majority of deaths from prostate cancer are attributed to the incurable, late stage cancer form and metastasis of the primary tumor. Due to the significant mortality and morbidity rate associated with the progression of this disease, there is an urgent need for new and targeted treatments. Generally, prostate cancer is an excellent target for targeted therapies. An important reason is a presence of specific surface proteins, glycoproteins, receptors, enzymes and peptides on the membrane of prostate cancer cells. One of these is the prostate specific membrane antigen. To date, several antibodies against this antigen have been developed and several targeted therapy approaches were investigated with these antibodies. Experimental therapies with drugconjugated, immunotoxin-conjugated and vaccine-conjugated antibodies have yielded objective clinical responses, however, they were observed in a minor fraction of patients and at doses near the maximum tolerated dose because of their toxicity and immunogenicity. These obstacles can potentially be overcome by designing radio-immunoconjugates for targeted radionuclide therapy. Targeted radionuclide therapy has the advantage of delivering a highly concentrated absorbed dose to the targeted tumor while sparing the surrounding normal tissues. In addition, the selective ability of radionuclide therapy is advantageous in the treatment of systemic malignancy, such as in bone metastases, where whole body irradiation using external beam radiotherapy is impossible. Since the administration of radionuclides is minimally invasive and the duration of treatment is shorter than chemotherapy, targeted radionuclide therapy has become one of the most preferred types of cancer therapy. For therapeutic purposes, β-particles and α-particles are preferable. However, recently many studies showed that effectiveness of therapy with β-emitters is not optimal for prostate cancer treatment and that α-emitters are the most preferred agents. Taking this into account, we propose pioneering approach which consists in using new compound (based on antibody conjugated nanomaterials labeled with alpha-emitter) as a potential radiopharmaceutical for targeted therapy of prostate cancer. The main objectives of the project are: (1) analysis of toxicity of unlabeled antibodyconjugated nanomaterials as carriers in vitro, (2) analysis of efficacy of antibody-conjugated nanomaterials labeled with α-emitter in vivo and (3) analysis of biodistribution and efficacy of this compound in vivo. In vitro experiments will be performed on human cancer and normal prostate cells. In vivo experiments will be performed on a mice model with tumors containing human prostate tumor cells. This interdisciplinary project involves chemical and physicochemical methods as well as quantitative and qualitative biological methods, including molecular biology methods, cell biology methods and immunological methods. The results which will be obtained from planned experiments will make an important contribution to the knowledge about new nanostructure-based radio-bioconjugates for targeted cancer therapy.